Urology and Male Reproductive Health
At our Fertility Center, we care for the health of both women and men. Our clinic has a urologist-andrologist who specializes in diagnosing and treating male reproductive disorders and urinary tract conditions.
A consultation with a urologist is recommended for men who are experiencing:
- Infertility or poor sperm quality
- Erectile dysfunction or other sexual health issues
- Urination problems
- Inflammation or pain in the genital area
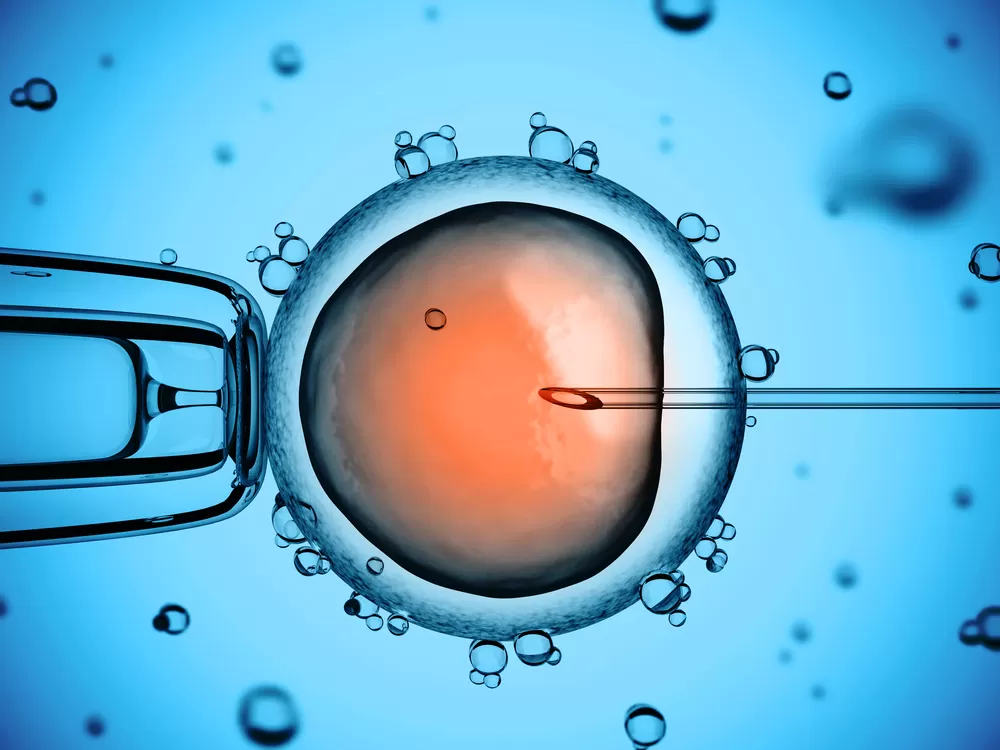
Semen Analysis (Spermogram)
One of the primary methods for assessing male fertility is a semen analysis, which evaluates key sperm quality indicators:
- Sperm concentration
- Motility (movement)
- Morphology (percentage of normal-shaped sperm)
- Signs of infection
The sample is collected via masturbation.
To ensure accurate results, we recommend 2–3 days of sexual abstinence before the test.
Results are available the same day, and our embryologist will explain them in detail over the phone.
MiOXSYS Test – Oxidative Stress Assessment
This innovative test evaluates oxidative stress in semen, one of the major — and often overlooked — causes of male infertility.
Scientific research has shown that 25–40% of male infertility cases are idiopathic (of unknown cause) and are strongly associated with oxidative damage to sperm.
That’s why it’s essential to assess not only standard sperm parameters, but also the level of oxidative stress to determine the root cause and choose the most effective treatment.
At our center, men receive confidential, professional, and compassionate care.
We are here to support every couple in their journey toward achieving their dream of becoming parents.